







An allergy, or hypersensitivity, is an overreaction of the immune system that occurs as a result of the body’s contact with an allergen.
This hypersensitivity may contribute to the development of serious diseases, such as: allergic rhinitis (AR), allergic asthma, atopic dermatitis (AD), and allergic conjunctivitis.
of preschool and school‑aged children suffer from allergies
Inhalant allergy (also known as respiratory allergy) is the most common type of allergy worldwide.
It occurs when airborne allergens enter the body through the respiratory tract, triggering the immune system in susceptible individuals.
Everyday environments are full of potential triggers, and prolonged exposure to them can lead to bothersome symptoms.
The group of allergens most commonly causing inhalant allergy includes:
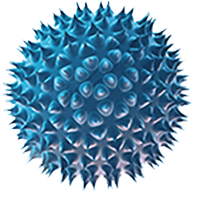
House dust mites are tiny arachnids belonging to the Pyroglyphidae family. Adult body length does not exceed 0.35 mm. The humidity and temperature conditions, along with the availability of food in sleeping areas, mean that the largest number of mites and their associated allergens are found in mattress dust. The most commonly encountered species are Dermatophagoides pteronyssinus and D. farinae. Allergens found in the fecal particles of these mites, designated Der p 1 and Der f 1, have strong sensitizing properties and are recognized as the most frequent cause of dust allergy, including allergic asthma.
– is mostly present in spring and autumn. It appears both outdoor and indoor. When pollen interacts with rhinitis or pharyngeal mucosa, it may cause multi-organ ailments of eyes, skin, mouth or throat.
– it is another group of allergens. The main source of them are proteins coming from pets’ saliva, skin and urine. Contrary to some common opinions, pets’ hair very rarely plays the role of an allergen. It is though a very good mean of transport for the allergens coming from sweat glands, saliva and urine.
– are one of the biggest groups of living organisms. The parts of fungi, such as fungal spores or the elements of mycete can cause allergic ailments and the development of the disease. Fungi allergy usually co – exists with the sensitiveness to other aeroallergens, mainly pollen and house-dust allergens.
Although sensitivity to house dust mites is year‑round in nature, a diagnostic indication is an exacerbation of the condition. It typically occurs in the morning and at night, most often in autumn and winter (during the heating season). A linear relationship has been demonstrated between the risk of asthma symptoms and the concentration of the main Dermatophagoides pteronyssinus allergen (Der p1) in house dust – the risk doubles with every doubling of the Der p1 concentration in the range of 0.7 to 50 mg per gram of dust.
Roll up Unroll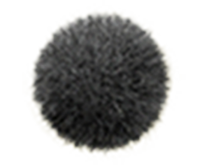

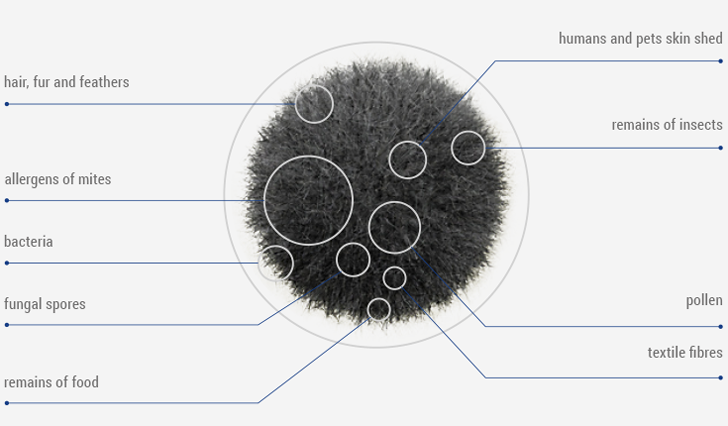
Household dust is the most common factor causing allergic reactions. It contains nearly all allergens present at home, such as allergens of pets, molds and plant pollens.
It is recommended to spray those areas in the home where the concentration of house dust allergens is highest. In particular mattresses, beds and other sleeping areas, duvets and pillows, upholstered furniture, carpets, rugs, curtains, and plush toys.

Symptoms develop as a result of inhalation of allergens by a sensitized person. Within a few minutes of contact with an allergen, a runny nose with watery discharge, impaired nasal airflow (a sensation of nasal congestion), itching, and sneezing occur. There is also a risk of acute and chronic sinusitis. The severity of symptoms depends on individual characteristics of the allergic person and the concentration of allergens in the home.
In severe cases of chronic allergic rhinitis, sleep disturbances, limitations in daily physical activity, and difficulty concentrating on studying and work may occur. A typical feature of AR is year‑round symptoms due to continuous exposure to household allergens.
To distinguish this type of allergy from a common cold caused by viral infection, attention should be paid to the duration of symptoms. Viral rhinitis usually lasts up to 10 days.
Allergic rhinitis is the most common non‑infectious disease of the upper respiratory tract, and it has been found in 36% of those studied (source: ECAP – Epidemiology of Allergic Diseases in Poland). AR may occur together with other allergic diseases such as asthma, allergic conjunctivitis, and atopic dermatitis.

Atopic dermatitis, also known as atopic eczema, is the most common skin disease whose first symptoms usually appear in early childhood. The condition is chronic with characteristic flare‑ups. It is estimated that between 1.5 and 2.5 million people in Poland suffer from AD, including 1–3% of adults.
The condition results from a genetically determined abnormal structure of the skin barrier. A deficiency of free fatty acids at this site facilitates allergen penetration, which leads to increased inflammation and itching. The epidermis is dry and thickened. AD may occur together with other allergic diseases such as asthma, allergic rhinitis, urticaria, and food allergy.
Key symptoms include itching, dry skin, inflammatory lesions resembling eczema, and thickening of the epidermis (lichenification). The epidermis of people with AD has a reduced content of ceramides and free fatty acids. As a result, the skin’s ability to bind water decreases, leading to faster evaporation. Elasticity decreases, making the skin more susceptible to micro‑injuries and cracking.
The disease may occur simultaneously with other atopic conditions such as asthma, allergic rhinitis of the upper respiratory tract, urticaria, and food allergy. Environmental factors important in the development and exacerbation of atopic dermatitis include household allergens such as dust mites, animal dander and hair, mold spores, and plant pollens, as well as foods. These allergens exhibit strong sensitizing properties upon contact with a susceptible person.
Roll up UnrollIts symptoms manifest themselves immediately after birth – skin becomes dry or there are skin lesions, such as erythema or exudate. They are located mainly near elbows and knee creases.
The dryness of the epidermis is accompanied by exfoliation and roughness. Skin thickens in the skin folds and on the forehead. On the elbows and knee creases there are alveolar-follicular lesions.
In adult patients, skin lesions are usually present at elbows and knee creases and at the base of the neck. The lesions can cover a large part of the body and they usually are more visible on the neck and face.

The presence of allergens in the home (including house dust mite allergens) can cause chronic bronchial inflammation. Those affected experience episodes of shortness of breath, coughing, wheezing, and increased mucus production. Narrowing of airflow through the bronchi under the influence of environmental factors is called bronchial hyperreactivity. This is characteristic of asthma.
In recent years, an increase in the number of people with asthma has been observed. Epidemiological studies published recently have shown asthma in 11% of children and 9% of adults in Poland. These figures may actually be higher due to difficulties in diagnosing the disease. Co‑occurrence of asthma, rhinitis, and atopic dermatitis is also noted, especially in childhood. (Polish Allergology, 2014)
Roll up UnrollEnvironmental factors promoting asthma development:

Asthma is a disease with a variable course; it may be chronic or seasonal, related to physical exertion, environmental influences, or be a side effect of certain medications. In each case, the disease may vary in severity — mild, moderate, or severe.
An important element of its prevention and treatment (as well as other allergic conditions) is the elimination of allergens from the environment. Effective measures can alleviate symptoms and decrease the risk of disease exacerbations. Additionally, removing allergens can protect individuals with atopic tendencies from the development of allergic disease.
Roll up UnrollVariable and reversible airflow limitation through the bronchi, called bronchial hyperresponsiveness, is a typical symptom of asthma. It occurs spontaneously, but also under the influence of physical, chemical or biological agents.
Sometimes symptoms become exacerbated. They are characterized by increased dyspnoea, escalating cough, wheezing, chest tightness, which may impair lung function.
Chronic inflammation leads to the pathological repair processes, that is remodelling of tissues, which aggravate respiratory dysfunction. Bronchial smooth muscle contraction, mucosal oedema and overproduction of thick mucus take place during an asthma attack. Patients then feel a transient chest tightness.
While diagnosing asthma, physician recognises symptoms typical for this disease. Specialised tests, which reveal limited airflow through the airways are performed. Examination of tissues located in the bronchi acquired during biopsy has significant value during diagnostic process.

ELIMINATION OF ALLERGENS FROM THE ENVIRONMENT